Skarekrow
~~DEVIL~~
- MBTI
- Ni-INFJ-A
- Enneagram
- Warlock
Interesting.
Media personality Connie Willis was late for a meeting at Disney’s Celebration community in Florida, and hopelessly lost as she drove the confusing maze of streets and highways around Walt Disney World. Growing anxious because the meeting was important to her, Connie heard a voice in her head say “turn left.”
As someone who was open to paranormal phenomena (she's now weekend host of a popular nighttime radio show that covers the paranormal), Connie listened to that voice and quickly found her way to the meeting.
Years later, describing the experience, Connie said, “When you tell people you hear a voice, you worry that people will think you're schizophrenic, but every time I’ve heard something it has been 100 percent correct.”
It turns out that a lot of people would not think Connie was crazy for hearing a voice—possibly from a helpful spirit—because, according to Huffington Post/YouGov and Pew Research polls, a majority (up to 65 percent) of American’s believe in paranormal/supernatural phenomena that include spiritual energy, ghostly encounters, premonitions and connecting with the dead.

Moreover, a 2017 Chapman University survey found that a whopping 75 percent of Americans hold at least one paranormal belief, the most common beliefs being that ancient civilizations such as Atlantis once existed or that ghosts are real.
Despite the wide prevalence of beliefs in the paranormal, it’s hard to find any “hard” scientist—the kind who require hard evidence in tightly controlled studies—who take the paranormal seriously.
And indeed, I count myself among those hard scientists who remain highly skeptical of reports of ghosts, premonitions, aliens, lost continents, or past lives.
But, although I see little hard evidence for paranormal or supernatural phenomena, I also believe that conscientious scientists need to keep an open mind, and be very careful not to label things as “impossible.”
Reputable 19th century physicians and scientists thought it impossible that invisible particles (bacteria) could cause disease, and, over a century later, similarly reputable physicians and scientists thought it impossible that bacteria could cause ulcers, until Dr. Barry Marshall got the Nobel prize for proving that H. pylori bacteria actually do cause ulcers.
Similarly, physicist Eric Betzig recently got the Nobel prize for demonstrating a phenomenon that was widely believed to be impossible (overcoming something called the diffraction limit that restricts how much magnification is possible in a light microscope).
Finally, as I mentioned in my last post on Quantum Neuroscience, even a genius like Einstein turned out to be wrong when he labeled the quantum phenomenon “spooky action at a distance” impossible.
OK.
So keeping an open mind is important in science: but is there any hard scientific evidence for any paranormal phenomena?
Up until recently, I would have said such evidence was sketchy at best.
For example, in a previous post, Can your heart predict the future, I described research at Florida Atlantic University suggesting that changes in heart rate can sometimes foretell near-future events, but these findings remain highly controversial and are not widely accepted.
However last month, as my wife, Dr. Chris Gilbert, and I were researching new findings in mind-body medicine, we stumbled upon research in a new field called epigenetics that made me wonder whether a particular paranormal phenomena—memories from past lives—might not have at least a little bit of validity.
As opposed to the field of genetics, which concerns itself with studying the way changes in inherited genes influence anatomy, physiology and behavior of living organisms, epigenetic science explores ways that inherited genes are turned on or off.
For example, young mice who undergo early trauma undergo epigenetic changes in the way that gluco-corticoid receptor genes express themselves, making the traumatized animals more likely to develop stress hormone-related behavioral responses—such as social avoidance—later in life.
These epigenetic changes are thought to occur through processes such as methylation, in which a methyl group (CH4) attached to a DNA molecule prevents expression of a particular gene.
Although conventional wisdom held that such epigenetic changes to behavior stay with an individual and do not pass down to their progeny, studies conducted in 2016 suggest that acquired traits can indeed be passed down through the generations, even in humans.
Dr Nicola Iovino of the Max Planck Institute of Immunobiology and Epigenetics, a leading researcher in behavioral epigenetic said, "Epidemiological studies revealed a striking correlation between the food supply of grandfathers and an increased risk of diabetes and cardiovascular disease in their grandchildren."
A 2015 review article by Dr. Brian Dias of Emory University Medical School on trans-generational learning through epigenetics in the journal, Trends in Neuroscience, described additional evidence that learnings and experiences of ancestors can be passed down to human descendants, including, transmission of PTSD and anxiety/depression from parents to their children.
Animal research cited by Dr. Dias demonstrates that it’s even possible for memories, such as fear of specific odors, to be passed from parents to their offspring.
Could experiences and learnings of your parents and ancestors explain phenomena such as deja vu, intuition or even why you pick up math or music skills so quickly?
Did what happened to your ancestors directly influence your dreams, your memories or your emotions?
In this hard scientist’s opinion, recent research has moved the answer to such questions from a firm “No” to a definite “Maybe,” although I’m still trying to figure out whether I believe that all on my own, or got the belief—through the magic of epigenetics—from my parents.
Or grandparents.
Or great-grandparents.
The Paranormal:
Can New Science Explain Old Phenomena?
The new field of Epigenetics transforms the impossible into the possible.

Posted Jan 21, 2019
Can New Science Explain Old Phenomena?
The new field of Epigenetics transforms the impossible into the possible.
Posted Jan 21, 2019
Media personality Connie Willis was late for a meeting at Disney’s Celebration community in Florida, and hopelessly lost as she drove the confusing maze of streets and highways around Walt Disney World. Growing anxious because the meeting was important to her, Connie heard a voice in her head say “turn left.”
As someone who was open to paranormal phenomena (she's now weekend host of a popular nighttime radio show that covers the paranormal), Connie listened to that voice and quickly found her way to the meeting.
Years later, describing the experience, Connie said, “When you tell people you hear a voice, you worry that people will think you're schizophrenic, but every time I’ve heard something it has been 100 percent correct.”
It turns out that a lot of people would not think Connie was crazy for hearing a voice—possibly from a helpful spirit—because, according to Huffington Post/YouGov and Pew Research polls, a majority (up to 65 percent) of American’s believe in paranormal/supernatural phenomena that include spiritual energy, ghostly encounters, premonitions and connecting with the dead.

Moreover, a 2017 Chapman University survey found that a whopping 75 percent of Americans hold at least one paranormal belief, the most common beliefs being that ancient civilizations such as Atlantis once existed or that ghosts are real.
Despite the wide prevalence of beliefs in the paranormal, it’s hard to find any “hard” scientist—the kind who require hard evidence in tightly controlled studies—who take the paranormal seriously.
And indeed, I count myself among those hard scientists who remain highly skeptical of reports of ghosts, premonitions, aliens, lost continents, or past lives.
But, although I see little hard evidence for paranormal or supernatural phenomena, I also believe that conscientious scientists need to keep an open mind, and be very careful not to label things as “impossible.”
Reputable 19th century physicians and scientists thought it impossible that invisible particles (bacteria) could cause disease, and, over a century later, similarly reputable physicians and scientists thought it impossible that bacteria could cause ulcers, until Dr. Barry Marshall got the Nobel prize for proving that H. pylori bacteria actually do cause ulcers.
Similarly, physicist Eric Betzig recently got the Nobel prize for demonstrating a phenomenon that was widely believed to be impossible (overcoming something called the diffraction limit that restricts how much magnification is possible in a light microscope).
Finally, as I mentioned in my last post on Quantum Neuroscience, even a genius like Einstein turned out to be wrong when he labeled the quantum phenomenon “spooky action at a distance” impossible.
OK.
So keeping an open mind is important in science: but is there any hard scientific evidence for any paranormal phenomena?
Up until recently, I would have said such evidence was sketchy at best.
For example, in a previous post, Can your heart predict the future, I described research at Florida Atlantic University suggesting that changes in heart rate can sometimes foretell near-future events, but these findings remain highly controversial and are not widely accepted.
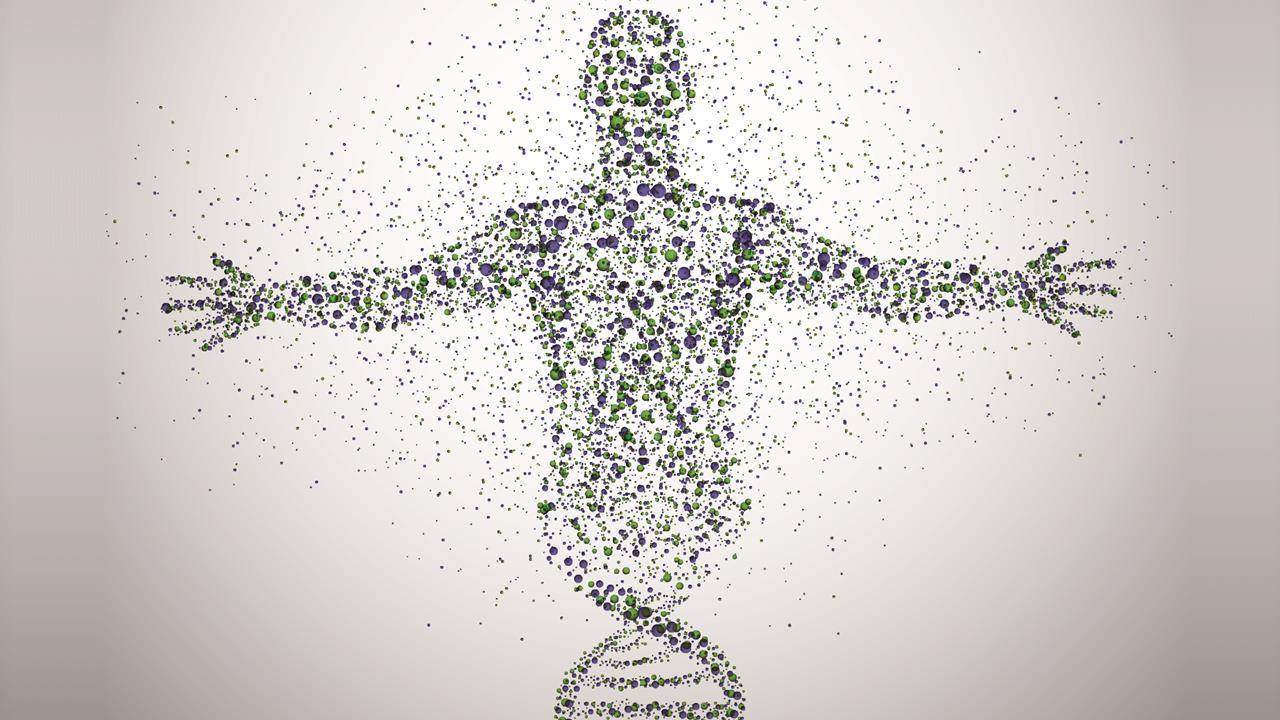
However last month, as my wife, Dr. Chris Gilbert, and I were researching new findings in mind-body medicine, we stumbled upon research in a new field called epigenetics that made me wonder whether a particular paranormal phenomena—memories from past lives—might not have at least a little bit of validity.
As opposed to the field of genetics, which concerns itself with studying the way changes in inherited genes influence anatomy, physiology and behavior of living organisms, epigenetic science explores ways that inherited genes are turned on or off.
For example, young mice who undergo early trauma undergo epigenetic changes in the way that gluco-corticoid receptor genes express themselves, making the traumatized animals more likely to develop stress hormone-related behavioral responses—such as social avoidance—later in life.
These epigenetic changes are thought to occur through processes such as methylation, in which a methyl group (CH4) attached to a DNA molecule prevents expression of a particular gene.
Although conventional wisdom held that such epigenetic changes to behavior stay with an individual and do not pass down to their progeny, studies conducted in 2016 suggest that acquired traits can indeed be passed down through the generations, even in humans.
Dr Nicola Iovino of the Max Planck Institute of Immunobiology and Epigenetics, a leading researcher in behavioral epigenetic said, "Epidemiological studies revealed a striking correlation between the food supply of grandfathers and an increased risk of diabetes and cardiovascular disease in their grandchildren."
A 2015 review article by Dr. Brian Dias of Emory University Medical School on trans-generational learning through epigenetics in the journal, Trends in Neuroscience, described additional evidence that learnings and experiences of ancestors can be passed down to human descendants, including, transmission of PTSD and anxiety/depression from parents to their children.
Animal research cited by Dr. Dias demonstrates that it’s even possible for memories, such as fear of specific odors, to be passed from parents to their offspring.
Could experiences and learnings of your parents and ancestors explain phenomena such as deja vu, intuition or even why you pick up math or music skills so quickly?
Did what happened to your ancestors directly influence your dreams, your memories or your emotions?
In this hard scientist’s opinion, recent research has moved the answer to such questions from a firm “No” to a definite “Maybe,” although I’m still trying to figure out whether I believe that all on my own, or got the belief—through the magic of epigenetics—from my parents.
Or grandparents.
Or great-grandparents.